What Childhood Food Allergies Really Are
A handful of foods are responsible for most allergic reactions in children. The usual suspects? Milk, eggs, peanuts, tree nuts, soy, wheat, fish, and shellfish. These eight are labeled as major allergens for a reason they account for around 90% of all food allergy cases in kids.
What happens inside the body is pretty basic, if a bit dramatic: the immune system misidentifies a harmless food protein as a threat. In response, it releases chemicals like histamine, which cause symptoms ranging from a rash to difficulty breathing. It’s your kid’s immune system going full DEFCON 1 over a slice of bread or a spoonful of peanut butter.
An allergy is not the same as an intolerance. Allergies involve the immune system and can be life threatening. Intolerances are usually about digestion unpleasant, sure, but not dangerous. Lactose intolerance, for example, can lead to gas and cramping, while a milk allergy could trigger swelling or anaphylaxis. Big difference, and one that matters when you’re feeding a child.
Food allergies aren’t just inconvenient they can be serious. But knowing what you’re up against is the first step to managing it with confidence.
Spotting the Warning Signs Early
Food allergies can show up in a number of ways and they don’t always start with a dramatic reaction. It’s often the smaller signs that matter most early on.
Mild symptoms might include hives, itching, or a rash, especially around the mouth or hands. Some kids experience minor belly pain, nausea, or a few bouts of vomiting after eating certain foods. These reactions might not seem serious at first glance, but they’re often a clue your child’s immune system is responding to something it sees as a threat.
Moderate symptoms can involve more intense skin outbreaks, ongoing stomach cramps, or diarrhea. You might notice your child becoming unusually tired or irritable after a meal. Take these signs seriously they can escalate or repeat.
Severe allergic reactions usually hit fast. Watch for swelling in the face, lips, or tongue, trouble breathing, wheezing, or a sudden drop in blood pressure. These symptoms point to anaphylaxis, a life threatening condition that requires immediate attention.
If your child ever has trouble breathing, loses consciousness, or shows rapid swelling after eating something, don’t wait call emergency services and use an epinephrine auto injector if prescribed. Quick action can save lives.
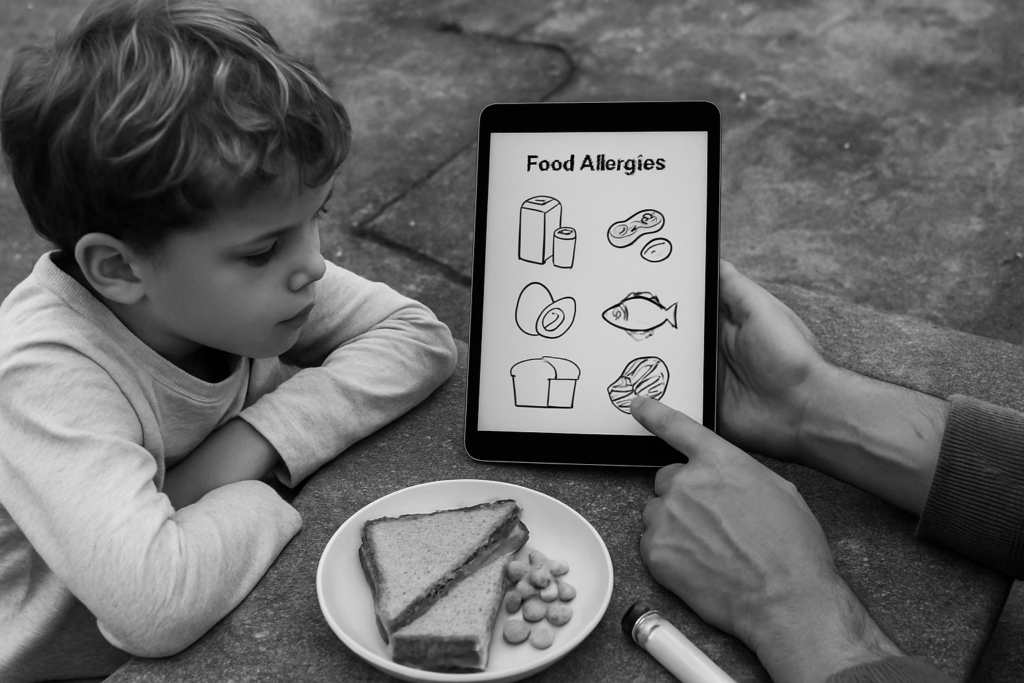
Diagnosing and Confirming Food Allergies
Getting to the bottom of a suspected food allergy starts with testing and observation, not guesswork. Skin prick tests and blood tests are the first tools doctors use. They’re quick, relatively painless, and help identify the specific allergens your child might be reacting to. But keep in mind, these tests don’t give a full picture on their own they point to sensitization, not always actual allergic reactions.
That’s where the elimination diet comes in. This is a careful process of removing potential allergens from your child’s meals and then slowly reintroducing them one at a time. It takes patience, sometimes weeks, and a solid food diary. Tracking symptoms closely everything from skin changes to moods can reveal cause and effect patterns that tests alone can miss.
All of this should be done under the guidance of a pediatric allergist. Their job isn’t just diagnostics, but helping you avoid false positives and unneeded restrictions. They’ll help you design a safe testing approach and adjust as needed. When done right, this process doesn’t just pinpoint the problem it lays the groundwork for long term allergy management with confidence, not constant fear.
Practical Steps for Managing Allergies

Managing food allergies well isn’t just about avoiding peanuts it’s about staying sharp, day in and day out. It starts at the grocery store. Reading labels like a pro means more than just spotting bolded allergens. You’ve got to look closely at ingredient lists for hidden terms, watch for “made in a facility with” warnings, and know that formulations can change without notice. Re check labels even on trusted brands. Nothing gets a free pass.
Next, your kitchen needs to run as a controlled zone. Separate utensils, cookware, cutting boards all of it. Cross contamination happens fast and doesn’t need much to trigger a reaction. One sponge touched by peanut butter and rubbed on a plate? That’s enough. Keep surfaces clean, prep allergen free meals first, and store allergy safe food in separate, clearly marked containers.
But safety doesn’t stop at home. Kids go to school. They get invited to birthday parties and sleepovers. That’s where communication matters. Be upfront and specific with teachers, coaches, and other parents. Provide a plan, backup snacks, and any medication your child might need. It’s not about being overprotective it’s about setting clear boundaries. When people understand the why, they’re more likely to support your child’s needs. And your child watches how you handle it so lead with confidence, not fear.
Creating a Supportive Daily Routine
Helping your child live with food allergies goes beyond managing ingredients it’s about fostering confidence, belonging, and a support system that empowers them.
Prioritizing Emotional Support
Living with food allergies can make children feel different or excluded. Emotional well being plays a vital role in how they manage their condition.
Validate their feelings when they feel left out or frustrated
Encourage open conversations about their allergies and any fears they may have
Involve them in safe meal planning to give them a sense of control
Fostering Inclusion
Inclusivity matters children thrive when they feel part of the group. You can help ensure they’re never left out during meals, playdates, or birthday parties.
Provide allergy safe snacks or treats for classroom parties
Work with teachers to ensure your child is included in activities without being singled out
Role play common situations (like sharing food or being offered a snack) so your child knows how to respond confidently
Educating the Inner Circle
Everyone who spends time around your child should know how to support their safety.
Train siblings to recognize symptoms and avoid sharing unsafe foods
Discuss what allergy friendly behavior looks like with babysitters and extended family
Share your child’s allergy action plan with any regular caregivers
Packing Allergy Friendly Lunches
Lunchtime at school can be one of the trickiest parts of the day. A little planning can go a long way in making it safe and enjoyable.
Create a rotating menu of allergy safe meals so your child feels excited and not restricted
Use containers to keep foods separated and avoid potential cross contact
Include a fun note or familiar treat to help your child feel connected to home during the day
Supporting a child with food allergies takes care, planning, and communication but with a strong routine in place, it becomes second nature for the entire family.
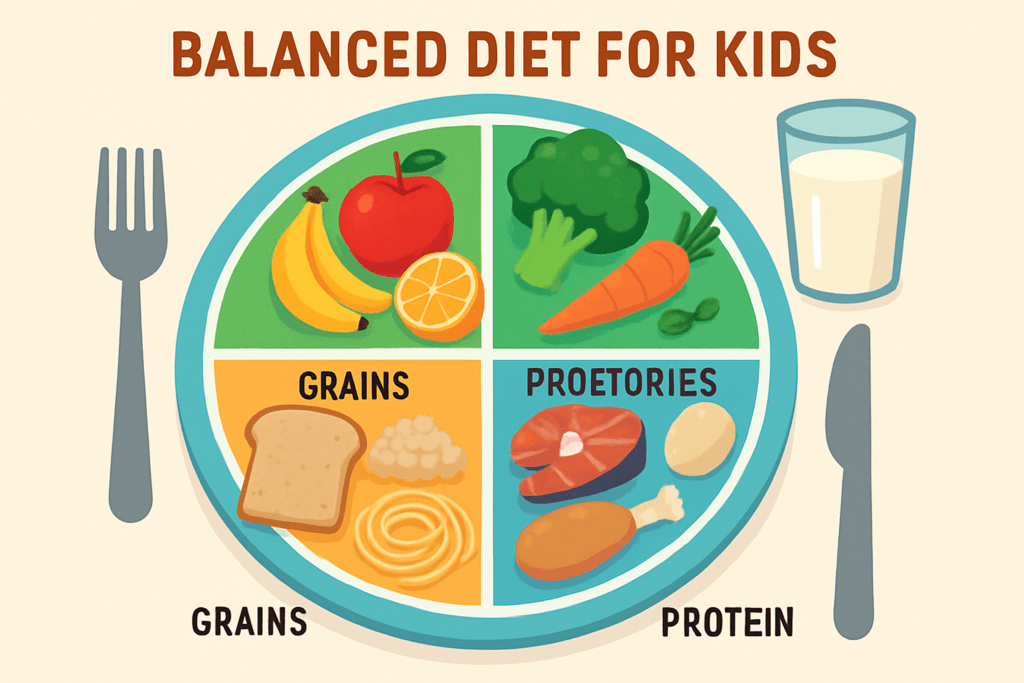
Nutrition Without the Risk
Feeding a child with food allergies can feel like solving a puzzle, but it’s doable and essential. The goal stays simple: deliver all the nutrients they need, minus the ingredients that put them at risk. That starts with having a clear understanding of what to swap and how to build meals that hit the mark on protein, fats, carbs, vitamins, and minerals.
For example, if dairy is off the table, fortified plant based milks (like oat or soy) can help cover calcium and vitamin D. Egg substitutes vary depending on use: flaxseed, chia, or commercial egg replacers work for baking; tofu or avocado can fit into breakfast. Can’t do nuts? Seeds like pumpkin and sunflower slide in nicely for snacks and added fats.
The smartest move is building a rotating menu full of whole foods fruits, veggies, lean proteins, grains and testing substitutions that work for your kid’s taste and tolerance. Processed “free from” products help in a pinch, but long term balance comes from real food.
Get the basics right, and the long term benefits show up: stronger growth, improved immune response, fewer nutritional gaps, and less anxiety around food. Managing allergies well isn’t just about what not to eat it’s about giving your child a safe, nourishing foundation that lets them thrive.
More tips here on building a balanced diet for a child.
Emergency Readiness
An allergic reaction can escalate fast. Knowing when to use an epinephrine auto injector isn’t optional it’s life saving. If your child shows signs of anaphylaxis (trouble breathing, swelling of the face or throat, sudden drop in blood pressure), don’t hesitate. Use the auto injector immediately and call emergency services. Time matters more than second guessing.
Every adult who regularly interacts with your child teachers, coaches, babysitters needs hands on training. Watching a video isn’t enough. Practice with a trainer device. Know the steps. Know the signs. Refresh that training at least once a year.
Keep the allergy action plan updated and simple. One page, clear instructions, and placed where it’s easy to find: school nurse’s office, backpack, glove compartment. Make sure key people know exactly where to find it and what to do. Preparedness removes panic from the equation.
Empowering Your Child
Teaching your child to speak up about their food allergies isn’t just smart it’s essential. Depending on their age, kids can learn simple ways to tell others what they can and can’t eat. A younger child might just say, “I can’t have peanuts or I get sick.” Older kids should know how to ask about ingredients, read labels, or confirm what’s in food before they eat it.
Start with the basics early. Practice at home. Role play birthday parties, restaurant orders, or school lunch conversations. The goal isn’t to make them anxious, but to give them the language and confidence to protect themselves when you’re not around.
Confidence builds with repetition and support. A child who feels in control of their allergy is less likely to feel isolated or stressed in social settings. Keep the focus on what they can enjoy not just what they need to avoid. Give them the tools, show them how, and back them up. You’re raising an advocate, not a bystander.

 Health & Nutrition Editor
Health & Nutrition Editor