What Food Allergies Really Are
Understanding food allergies begins with knowing how they differ from food intolerances. Although they may share some symptoms, they involve different systems in the body and the consequences can be far more serious.
Food Allergy vs. Food Intolerance
Food allergy involves the immune system and can result in life threatening reactions, while food intolerance typically affects the digestive system and may cause discomfort but is rarely dangerous.
Key differences include:
Immune response vs. digestive response
Rapid onset (within minutes) in allergies vs. delayed symptoms in intolerances
Allergies often trigger symptoms like hives, swelling, or anaphylaxis
Intolerances may lead to bloating, gas, or stomach cramps
Most Common Food Allergens
There are eight primary foods responsible for the majority of serious allergic reactions in children:
Peanuts
Eggs
Cow’s milk (dairy)
Shellfish (e.g., shrimp, crab)
Tree nuts (e.g., walnuts, almonds)
Soy
Wheat
Fish (e.g., salmon, tuna)
Many children may outgrow allergies to milk, eggs, and soy, while others especially peanut and shellfish allergies tend to persist into adulthood.
What Happens in the Body
When a child with a food allergy consumes a trigger food, their immune system reacts as if it’s a harmful substance. This leads to the release of chemicals like histamine, which causes symptoms such as:
Swelling of the lips, face, or throat
Hives or skin rash
Nausea, vomiting, or diarrhea
Difficulty breathing
In severe cases, anaphylaxis can occur a fast moving, life threatening reaction that requires immediate medical attention.
Understanding how the immune system misidentifies certain foods as threats is key to preventing exposure and acting quickly when symptoms appear.
Early Warning Signs to Watch For
Food allergies don’t always start with drama. Sometimes, the first signs are easy to miss: a mild skin rash, a few extra trips to the bathroom, a fussy mood that feels off. These subtle symptoms red patches around the mouth, bloating, irritability can wave the first red flags that something in your child’s diet isn’t being welcomed by their immune system.
But the shift from subtle to serious can happen fast. Swelling of the lips or face, persistent vomiting, difficulty breathing or wheezing these are not wait and see moments. These are medical emergencies. And they can happen within minutes of eating the wrong thing.
When you see your child struggling to breathe, swelling up rapidly, or vomiting uncontrollably, call emergency services without hesitation. Time is everything in these situations.
If you’re unsure whether a reaction is serious, err on the side of caution. Keep an allergy action plan handy and walk through it step by step. Knowing when to act is half the battle when it comes to food allergies.
Prevention Begins with Smart Feeding Habits

For a long time, the advice was to delay introducing common allergens like peanuts or eggs. Today, research says the opposite. Multiple studies including the LEAP (Learning Early About Peanut Allergy) trial now show that introducing allergens early, between 4 and 11 months, can actually lower the risk of developing food allergies. In plain terms, avoiding triggers isn’t the strategy anymore. Controlled exposure is.
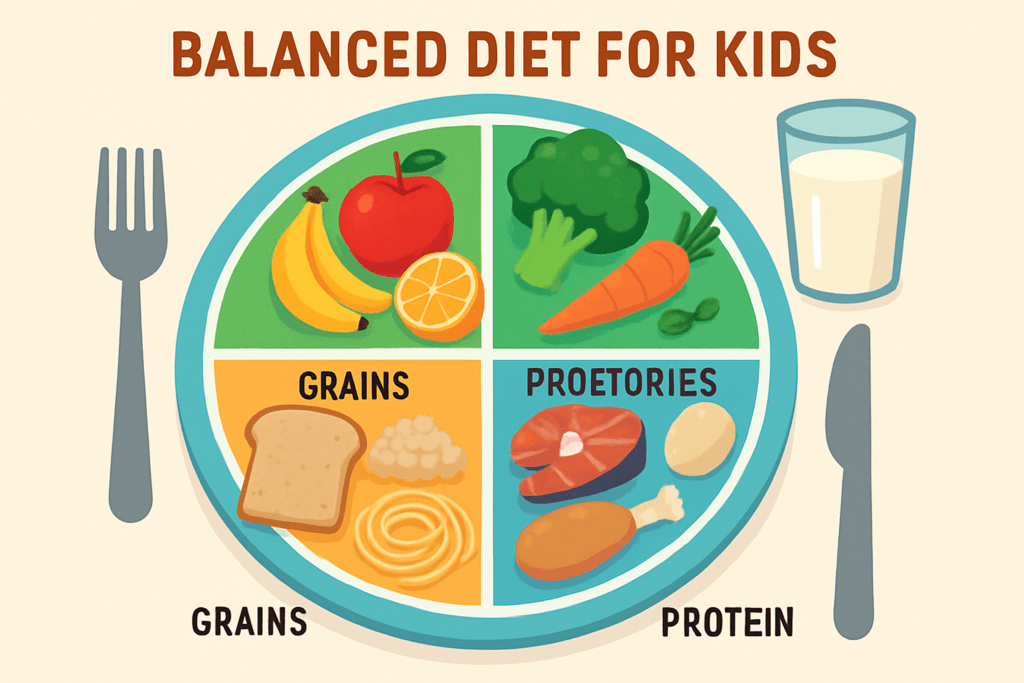
Variety also plays a key role. Offering a mix of safe, age appropriate foods not only supports nutrition but helps train your baby’s immune system to tolerate a wider range of proteins. Rotating ingredients, rather than sticking to the same handful, builds resilience.
At home, stick with simple ingredients and avoid pre packaged meals with mystery contents. If your child eats at daycare or school, communication is key. Share ingredient lists, make caregivers allergy aware, and pack safe, labeled snacks when the menu looks suspect.
For more on how to build a balanced, allergy smart diet, check out this guide.
Nutrition Tips to Support Immunity
When it comes to preventing food allergies, nutrition plays a bigger role than most parents realize. A child’s immune system is shaped early, and the gut is ground zero. That’s where probiotics come in. Found in fermented foods like yogurt or available in supplement form, probiotics help balance gut bacteria and may reduce the likelihood of allergic reactions. Think of them as quiet bodyguards for your child’s digestion supportive, subtle, and always working behind the scenes.
Vitamin D is another heavyweight. Most kids don’t get enough, especially in the colder months. Low levels have been linked to increased allergy risks. A simple supplement or a bit more time outdoors can make a difference. Omega 3s those healthy fats found in fish, flaxseeds, and walnuts also help by calming inflammation and supporting overall immune response.
Then there’s breastfeeding. It’s not just bonding or basic nutrition. Breast milk contains immune boosting compounds that help protect against early onset allergies, especially when continued during the introduction of solid foods.
Bottom line: gut health, nutrition, and early feeding choices all stack the odds in your child’s favor. For a deeper look at what a balanced child diet actually includes, explore the fundamentals of a balanced child diet.
Partnering With Your Pediatrician
When it comes to navigating food allergies, guessing isn’t enough. This is where your pediatrician becomes a key player.
First up: allergy testing. If your child shows any symptoms rash, hives, trouble breathing, or even digestive issues after meals it’s time to talk testing. Skin prick tests or blood tests can help identify specific triggers. Some pediatricians may refer you to an allergist for a more detailed work up. It’s not about labeling your child with a list of allergies forever it’s about getting clear data so you can act with confidence.
Next comes the food introduction plan. This isn’t just about throwing peanuts into your kid’s lunch and hoping for the best. A smart plan involves slowly bringing in common allergens like eggs, dairy, and nuts, one at a time, and in tiny amounts especially if your child is high risk. Your pediatrician can help pace it out, tell you what signs to watch for, and decide whether any food challenges should happen under medical supervision.
Then there’s the just in case gear: the epinephrine auto injector. If your child has a diagnosed allergy especially one that caused a moderate or severe reaction you may need to carry one. It’s not overkill; it’s planning for the worst while expecting the best. And yes, even older kids should learn when and how to use it.
Working closely with your pediatrician grounds your decisions in science, not internet panic. You’re not trying to control every bite your child eats you’re trying to help them thrive, safely.
Final Takeaways for Everyday Confidence
Navigating food labels isn’t rocket science, but it does take focus. Hidden allergens often show up under tricky names casein for dairy, albumin for eggs, or vague terms like “natural flavors” that may include soy or tree nuts. The golden rule: read the label twice. Once when you buy, and again before cooking. Labels change without warning. Get used to scanning for the top nine allergens and cross contamination disclaimers like “processed in a facility that also handles…”
Next step: teaching kids how to protect themselves. Start simple and early. Show them what their allergen looks like on a label. Practice role playing situations at school, a birthday party, asking a waiter about ingredients. The goal isn’t fear it’s awareness. The more confident they are, the more independent they become.
Finally, don’t let food allergies turn your family’s meals into a safety drill. Try new recipes. Travel with snacks you trust. Learn how to adapt classic dishes. With the right habits, your kitchen (and your kid’s taste buds) can stay open to exploration. Food safety doesn’t have to cancel food joy.































































 Senior Parenting Writer
Senior Parenting Writer